Lormetazepam, sold under the brand name Noctamid among others, is a drug which is a short to intermediate acting 3-hydroxy[3] benzodiazepine derivative and temazepam analogue.[4] It possesses hypnotic, anxiolytic, anticonvulsant, sedative, and skeletal muscle relaxant properties.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Noctamid, Loramet, others |
| Other names | Methyllorazepam; Methyl-lorazepam; N-Methyllorazepam; Ro 5-5516 |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Oral, intravenous[1] |
| Drug class | Benzodiazepine |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 80% |
| Metabolism | Hepatic |
| Elimination half-life | 10–12 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.011.546 |
| Chemical and physical data | |
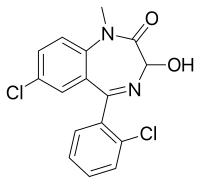
| Formula | C16H12Cl2N2O2 |
| Molar mass | 335.18 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
It was patented in 1961 and came into medical use in 1980.[5] Lormetazepam is not approved for sale in the United States or Canada. It is licensed in the UK as 0.5 and 1 mg tablets for short-term treatment (2–4 weeks) of moderately severe insomnia. It is licensed in the Netherlands as 1 and 2 mg tablets, under the brand names Loramet and Noctamid and as generic, available from several manufacturers. It is sold in Poland as Noctofer. It is also sold in France as generic as 1 and 2mg tablets, with a maximum prescription duration of 4 weeks. A Dutch analysis stated that lormetazepam could be suitable to be included in drug prescribing formularies, although zolpidem, zopiclone, and temazepam appear better.[6]
Medical uses
editLormetazepam is considered a hypnotic benzodiazepine and is officially indicated for moderate-to-severe insomnia. Lormetazepam is a short-acting benzodiazepine and is sometimes used in patients who have difficulty in maintaining sleep or falling asleep. Hypnotics should only be used on a short-term basis or, in those with chronic insomnia, on an occasional basis.[7]
Side effects
editSide effects of lormetazepam are similar to those of other hypnotic benzodiazepines and can for the most part be regarded as a class effect.[citation needed] In a sleep study, 1 mg lormetazepam increased total sleep time, reduced wakefulness, but did not alter REM sleep. However, at 2 mg doses, there were significant increases in stage 3 sleep and reductions in REM sleep. Rebound effects have been reported after chronic use including rebound REM.[4] In one clinical trial with patients who had prior experience with older hypnotics temazepam and nitrazepam, most preferred lormetazepam due to less heavy sedation, amnesia, and residual effects.[8] Some side effects, including drowsiness, amnesia, and respiratory depression, are increased when lormetazepam is combined with other drugs with similar effects, e.g. alcohol and nonbenzodiazepine drugs.
Although lormetazepam has been associated with adversely affecting immediate and delayed recall memory functions,[9] studies have shown that lormetazepam's amnesic properties may be lesser compared to other hypnotic benzodiazepines. For example, in a 1984 study comparing the amnesic effects of lormetazepam to temazepam and flurazepam showed that amnesia was smallest after lormetazepam and greatest after temazepam, which had produced greater amnesia than both lormetazepam and flurazepam by a significant margin.[10]
Side effects of lormetazepam include:
- Somnolence
- Paradoxical increase in aggression
- Lightheadedness
- Confusion
- Muscle weakness
- Ataxia (particularly in the elderly)
- Anterograde amnesia
- Headache
- Vertigo
- Hypotension
- Salivation changes
- Gastrointestinal disturbances
- Visual disturbances
- Dysarthria
- Tremor
- Changes in libido
- Urinary incontinence
- Urinary retention
- Blood disorders and jaundice
- Skin reactions
- Dependence and withdrawal reactions
Residual "hangover" effects after nighttime administration of lormetazepam such as sleepiness, impaired psychomotor and cognitive functions may persist into the next day which may impair the ability of users to drive safely and increase risks of falls and hip fractures.[11]
Benzodiazepines require special precaution if used during pregnancy, in children, in alcohol- or drug-dependent individuals and individuals with comorbid psychiatric disorders.[12] Lormetazepam may be unsuitable for the elderly due to residual effects on memory and body sway which may result in falls.[13] Lormetazepam causes impaired driving skills, thus caution is required in individuals who drive or operate machinery.[14]
Tolerance, dependence, and withdrawal
editThe risks of tolerance, dependence, and withdrawal are very low when the drug is used for 2–4 weeks only, and lormetazepam is generally a safe and effective drug when used for no longer than 2–4 weeks. Some sleep disturbance in the form of rebound insomnia can, however, occur even after short-term usage of 7 days.[15] Those with a history of addiction may be at increased risk of problems of tolerance and dependence especially those with a past history of dependency on sedative hypnotic drugs.
Lormetazepam as with other benzodiazepines is generally only recommended for short-term use (2–4 weeks) due to tolerance and loss of efficacy. Tolerance to and loss of the sedative effects of benzodiazepine hypnotics can occur within 14 days of regular use.[16] Some studies however suggest such treatments retain their effectiveness in the long term[17][18][19] - such a lack of consistency in the findings of many studies could be due to the variation of responses to benzodiazepine treatment.
Dependence is the medical term for addiction. Dependence can either be psychological and/or physical. Psychological dependence can manifest itself as a reliance on a drug to cope with everyday life or in the form of craving. Physical dependence occurs due to physiological adaptations occurring as the body attempts to overcome the drugs effects which is known as tolerance and the continuing need to take the drug to avoid or suppress withdrawal symptoms which can sometimes resemble the original condition being treated. When the dose or the drug is discontinued withdrawal symptoms typically occur. Lormetazepam as with all other benzodiazepines produces both physical and psychological dependence but the main problem of concern is physical dependence which appears in the form of the benzodiazepine withdrawal syndrome after the dosage is reduced or the drug is stopped completely.[20] The dependence induced by lormetazepam is related to changes in the sensitivity of the GABA-BZD receptor complex.[21]
Withdrawal symptoms typically subside after 4–8 weeks but in approximately 10-15% of individuals symptoms can persist for many months[22] and in rare cases years.[23] Some "Withdrawal Symptoms" can emerge despite a constant dosage with the body needing extra dosage in order to feel normal. This is sometimes associated with dosage escalation.
Lormetazepam has a short to intermediate half-life of approximately 10–12 hours. Shorter acting benzodiazepine compounds are generally associated with a more intense and immediate withdrawal reaction compared to longer acting benzodiazepines. For this reason it is generally recommended to cross from lormetazepam to an equivalent dose of diazepam to gradually taper the dosage.[24]
Pharmacology
editThe bioavailability of lormetazepam was found to be 80%.[25]
Lormetazepam and other benzodiazepine drugs act as positive modulators at the GABAA benzodiazepine receptor complex. Lormetazepam binds to the benzodiazepine receptor which in turn enhances the effect of the GABAA receptor producing its therapeutic effects as well as adverse effects. When lormetazepam binds to the benzodiazepine receptor sites in sufficient quantities it produces sedation which is used clinically as a therapeutic treatment for insomnia. Lormetazepam alters the brain electrical activity which has been studied via EEG readings.[26] Lormetazepam appears to be more selective in the type of benzodiazepine receptor it binds to showing a higher affinity for the omega 1 receptor which is responsible for sedation.[27] Changes in EEG can therefore be used to measure the sedative sleep promoting properties of lormetazepam.
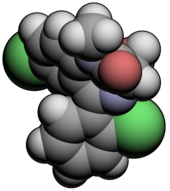
Chemistry
editStereochemistry
editLormetazepam has a stereocenter and two enantiomers. Medications are racemates.[28]
| Enantiomers of lormetazepam | |
|---|---|
| (R)-lormetazepam CAS number: 113679-56-4 |
(S)-lormetazepam CAS number: 113679-54-2 |
Industry
editBrand names
editTrade names include Aldosomnil, Dilamet, Ergocalm, Loramet, Loretam, Metatop, Minias, Noctamid, Noctamide, Noctofer, Nocton, Pronoctan, Sedaben, Sedalam, and Stilaze.
References
edit- ^ Horowski R (August 2020). "Dependence liability of lormetazepam: are all benzodiazepines equal? The case of the new i.v. lormetazepam for anesthetic procedures". Journal of Neural Transmission. 127 (8): 1107–1115. doi:10.1007/s00702-020-02209-8. PMC 8823007. PMID 32468272.
- ^ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ Doenicke A, Dorow R, Täuber U (December 1991). "[The pharmacokinetics of lormetazepam following cimetidine]" [The pharmacokinetics of lormetazepam following cimetidine]. Der Anaesthesist (in German). 40 (12): 675–679. PMID 1685875.
- ^ a b Nicholson AN, Stone BM (March 1982). "Hypnotic activity and effects on performance of lormetazepam and camazepam--analogues of temazepam". British Journal of Clinical Pharmacology. 13 (3): 433–439. doi:10.1111/j.1365-2125.1982.tb01398.x. PMC 1402107. PMID 6120717.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 537. ISBN 9783527607495.
- ^ Janknegt R, van der Kuy A, Declerck G, Idzikowski C (August 1996). "Hypnotics. Drug selection by means of the System of Objectified Judgement Analysis (SOJA) method". PharmacoEconomics. 10 (2): 152–163. doi:10.2165/00019053-199610020-00007. PMID 10163418.
- ^ Rickels K (1986). "The clinical use of hypnotics: indications for use and the need for a variety of hypnotics". Acta Psychiatrica Scandinavica. Supplementum. 332 (S332): 132–141. doi:10.1111/j.1600-0447.1986.tb08990.x. PMID 2883820. S2CID 46560074.
- ^ Hill RC, Harry TV (1983). "Lormetazepam (Lorámet): a multicentre assessment of its efficacy and acceptability as a hypnotic in out-patients with sleep disturbances". The Journal of International Medical Research. 11 (6): 325–332. doi:10.1177/030006058301100601. PMID 6360746. S2CID 23167620.
- ^ Dorow R, Berenberg D, Duka T, Sauerbrey N (1987). "Amnestic effects of lormetazepam and their reversal by the benzodiazepine antagonist Ro 15-1788". Psychopharmacology. 93 (4): 507–514. doi:10.1007/bf00207244. PMID 2893417. S2CID 1680477.
- ^ Roehrs T, McLenaghan A, Koshorek G, Zorick F, Roth T (1984). "Amnesic effects of lormetazepam". Sleep, Benzodiazepines and Performance. Psychopharmacology Supplementum. Vol. 1. pp. 165–72. doi:10.1007/978-3-642-69659-6_14. ISBN 978-3-642-69661-9. PMID 6147838.
- ^ Vermeeren A (2004). "Residual effects of hypnotics: epidemiology and clinical implications". CNS Drugs. 18 (5): 297–328. doi:10.2165/00023210-200418050-00003. PMID 15089115. S2CID 25592318.
- ^ Authier N, Balayssac D, Sautereau M, Zangarelli A, Courty P, Somogyi AA, et al. (November 2009). "Benzodiazepine dependence: focus on withdrawal syndrome". Annales Pharmaceutiques Françaises. 67 (6): 408–413. doi:10.1016/j.pharma.2009.07.001. PMID 19900604.
- ^ Allain H, Bentué-Ferrer D, Tarral A, Gandon JM (July 2003). "Effects on postural oscillation and memory functions of a single dose of zolpidem 5 mg, zopiclone 3.75 mg and lormetazepam 1 mg in elderly healthy subjects. A randomized, cross-over, double-blind study versus placebo". European Journal of Clinical Pharmacology. 59 (3): 179–188. doi:10.1007/s00228-003-0591-5. PMID 12756510. S2CID 13440208.
- ^ Staner L, Ertlé S, Boeijinga P, Rinaudo G, Arnal MA, Muzet A, Luthringer R (October 2005). "Next-day residual effects of hypnotics in DSM-IV primary insomnia: a driving simulator study with simultaneous electroencephalogram monitoring". Psychopharmacology. 181 (4): 790–798. doi:10.1007/s00213-005-0082-8. PMID 16025317. S2CID 26351598.
- ^ Kales A, Bixler EO, Soldatos CR, Mitsky DJ, Kales JD (12 November 1982). "Dose-response studies of lormetazepam: efficacy, side effects, and rebound insomnia". Journal of Clinical Pharmacology. 22 (11–12): 520–530. doi:10.1002/j.1552-4604.1982.tb02645.x. PMID 6131080. S2CID 694106.
- ^ Smith AE (1989). "Benzodiazepines - Use & Abuse - A Guide for Prescribers". New Zealand Department of Health.
- ^ Oswald I, French C, Adam K, Gilham J (March 1982). "Benzodiazepine hypnotics remain effective for 24 weeks". British Medical Journal. 284 (6319): 860–863. doi:10.1136/bmj.284.6319.860. PMC 1496323. PMID 6121605.
- ^ Vogel GW, Morris D (July 1992). "The effects of estazolam on sleep, performance, and memory: a long-term sleep laboratory study of elderly insomniacs". Journal of Clinical Pharmacology. 32 (7): 647–651. doi:10.1002/j.1552-4604.1992.tb05776.x. PMID 1640005. S2CID 44857913.
- ^ Walsh JK, Krystal AD, Amato DA, Rubens R, Caron J, Wessel TC, et al. (August 2007). "Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations". Sleep. 30 (8): 959–968. doi:10.1093/sleep/30.8.959. PMC 1978384. PMID 17702264.
- ^ Ashton CH (1995). "Protracted Withdrawal Symptoms From Benzodiazepines". Psychiatr Ann. 25: 158–165. doi:10.3928/0048-5713-19950301-09. Archived from the original on 21 August 2006.
- ^ Gerra G, Giucasto G, Zaimovic A, Fertonani G, Chittolini B, Avanzini P, et al. (June 1996). "Intravenous flumazenil following prolonged exposure to lormetazepam in humans: lack of precipitated withdrawal". International Clinical Psychopharmacology. 11 (2): 81–88. doi:10.1097/00004850-199611020-00002. PMID 8803645.
- ^ Ashton CH. "Benzodiazepines: How They Work And How To Withdraw".
- ^ Lader MH, Morton SV (January 1992). "A pilot study of the effects of flumazenil on symptoms persisting after benzodiazepine withdrawal". Journal of Psychopharmacology. 6 (3). Oxford, England: 357–63. doi:10.1177/026988119200600303. PMID 22291380. S2CID 23530701. Archived from the original on 11 June 2007.
- ^ "Benzodiazepines and Your Patients: A Management Programme". Roche Products (UK) Ltd. 1990.
- ^ Hümpel M, Stoppelli I, Milia S, Rainer E (1982). "Pharmacokinetics and biotransformation of the new benzodiazepine, lormetazepam, in man. III. Repeated administration and transfer to neonates via breast milk". European Journal of Clinical Pharmacology. 21 (5): 421–425. doi:10.1007/BF00542330. PMID 6122580. S2CID 19327058.
- ^ Kurowski M, Ott H, Herrmann WM (May 1982). "Relationship between EEG dynamics and pharmacokinetics of the benzodiazepine lormetazepam". Pharmacopsychiatria. 15 (3): 77–83. doi:10.1055/s-2007-1019513. PMID 6124982.
- ^ Ozawa M, Nakada Y, Sugimachi K, Akai T, Yamaguchi M (November 1991). "[Interaction of the hypnotic lormetazepam with central benzodiazepine receptor subtypes omega 1, omega 2 and omega 3]". Nihon Yakurigaku Zasshi. Folia Pharmacologica Japonica. 98 (5): 399–408. doi:10.1254/fpj.98.5_399. PMID 1687574.
- ^ Rote Liste Service GmbH (Hrsg.): Rote Liste 2017 – Arzneimittelverzeichnis für Deutschland (einschließlich EU-Zulassungen und bestimmter Medizinprodukte). Rote Liste Service GmbH, Frankfurt/Main, 2017, Aufl. 57, ISBN 978-3-946057-10-9, S. 196.
External links
edit- "Lormetazepam". Inchem.org.