Promethazine, sold under the brand name Phenergan among others, is a first-generation antihistamine, sedative, and antiemetic used to treat allergies, insomnia, and nausea. It may also help with some symptoms associated with the common cold[4] and may also be used for sedating people who are agitated or anxious, an effect that has led to some recreational use (especially with codeine).[5][6][7] Promethazine is taken by mouth (oral), as a rectal suppository, or by injection into a muscle (IM).[4]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Phenergan, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682284 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, rectal, intravenous, intramuscular, topical |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 88% absorbed but after first-pass metabolism reduced to 25% absolute bioavailability[2] |
| Protein binding | 93% |
| Metabolism | Liver glucuronidation and sulfoxidation |
| Elimination half-life | 10–19 hours[2][3] |
| Excretion | Kidney and Bile duct |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.445 |
| Chemical and physical data | |
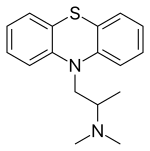
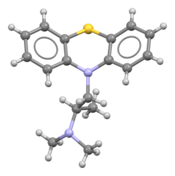
| Formula | C17H20N2S |
| Molar mass | 284.42 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Common side effects of promethazine include confusion and sleepiness;[4] consumption of alcohol or other sedatives can make these symptoms worse.[4] It is unclear if use of promethazine during pregnancy or breastfeeding is safe for the fetus.[4][6] Use of promethazine is not recommended in those less than two years old, due to potentially negative effects on breathing.[4] Use of promethazine by injection into a vein is not recommended, due to potential skin damage.[4] Promethazine is in the phenothiazine family of medications.[4] It is also a strong anticholinergic, which produces its sedative effects. This also means high or toxic doses can act as a deliriant.[8]
Promethazine was made in the 1940s by a team of scientists from Rhône-Poulenc laboratories.[9] It was approved for medical use in the United States in 1951.[4] It is a generic medication and is available under many brand names globally.[1] In 2022, it was the 198th most commonly prescribed medication in the United States, with more than 2 million prescriptions.[10][11] In 2022, the combination with dextromethorphan was the 260th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[10][12]
Medical uses
editPromethazine has a variety of medical uses, including:
- Sedation[13]
- In Germany, it is approved for the treatment of agitation and agitation associated with underlying psychiatric disorders with a maximum daily dose of 200 mg.[14]
- For nausea and vomiting associated with anesthesia or chemotherapy. It is commonly used postoperatively as an antiemetic. The antiemetic activity increases with increased dosing; however, side effects also increase, which often limits maximal dosing.[13]
- For moderate to severe morning sickness and hyperemesis gravidarum: In the UK, Promethazine is the drug of first choice. Promethazine is preferred during pregnancy because it is an older drug and there is more data regarding the use of it during pregnancy. Second choice medications, which are used if Promethazine isn't tolerated or the patient cannot take it, are metoclopramide or prochlorperazine.[15][13]
- For allergies such as hay fever and together with other medications in anaphylaxis[4]
- To aid with symptoms of the common cold[4]
- Motion sickness,[4] including space sickness[16]
- Hemolytic disease of the newborn[4]
- Anxiety before surgery[4]
- Short-term insomnia[17]
Side effects
editSome documented side effects include:
- Tardive dyskinesia, pseudoparkinsonism, acute dystonia (effects due to dopamine D2 receptor antagonism)[13]
- Confusion in the elderly[13]
- Drowsiness, dizziness, fatigue, more rarely vertigo
- Known to have effects on serotonin and dopamine receptors.[18]
- Dry mouth[13]
- Nausea[19]
- Respiratory depression in patients under age of two and in those with severely compromised pulmonary function[20]
- Blurred vision, xerostomia, dry nasal passages, dilated pupils, constipation, and urinary retention. (due to its anti-cholinergic effects)[13]
- Chest discomfort/pressure (In children less than 2 years old)[13]
- Akathisia[21]
Less frequent:
- Cardiovascular side effects to include arrhythmias and hypotension[13]
- Neuroleptic malignant syndrome[13]
- Liver damage and cholestatic jaundice[13]
- Bone marrow suppression, potentially resulting in agranulocytosis, thrombocytopenia, and leukopenia[13]
- Depression of the thermoregulatory mechanism resulting in hypothermia/hyperthermia[13]
Rare side effects include:
Because of potential for more severe side effects, this drug is on the list to avoid in the elderly.[22] In many countries (including the US and UK), promethazine is contraindicated in children less than two years of age, and strongly cautioned against in children between two and six, due to problems with respiratory depression and sleep apnea.[23]
Promethazine is listed as one of the drugs of highest anticholinergic activity in a study of anticholinergenic burden, including long-term cognitive impairment.[24]
Overdose
editPromethazine in overdose can produce signs and symptoms including CNS depression, hypotension, respiratory depression, unconsciousness, and sudden death.[25] Other reactions may include hyperreflexia, hypertonia, ataxia, athetosis, and extensor-plantar reflexes.[25] Atypically and/or rarely, stimulation, convulsions, hyperexcitability, and nightmares may occur.[25] Anticholinergic effects like dry mouth, dilated pupils, flushing, gastrointestinal symptoms, and delirium may occur as well.[25] Treatment of overdose is supportive and based on symptoms.[25]
Pharmacology
editPromethazine, a phenothiazine derivative, is structurally different from the neuroleptic phenothiazines, with similar but different effects.[2] Despite structural differences, promethazine exhibits a strikingly similar binding profile to promazine,[26] another phenothiazine compound. Both promethazine and promazine exhibit comparable neuroleptic potency, with a neuroleptic potency of 0.5.[27] However, dosages used therapeutically, such as for sedation or sleep disorders, have no antipsychotic effect.[28] It acts primarily as a strong antagonist of the H1 receptor (antihistamine, Ki = 1.4 nM[29]) and a moderate mACh receptor antagonist (anticholinergic),[2] and also has weak to moderate affinity for the 5-HT2A,[30] 5-HT2C,[30] D2,[31][32] and α1-adrenergic receptors,[33] where it acts as an antagonist at all sites, as well. New studies have shown that promethazine acts as a strong non-competitive selective NMDA receptor antagonist, with an EC50 of 20 μM;[34] which might promote sedation in addition with the strong antihistaminergic effects of the H1 receptor, but also as a weaker analgesic. It does not however affect the AMPA receptors.[34]
Another notable use of promethazine is as a local anesthetic, by blockage of sodium channels.[33]
| receptor | Ki (nM) | ref |
|---|---|---|
| α1A-adrenoceptor (Rat) | 32 | [35] |
| α1B-adrenoceptor (Rat) | 21 | [35] |
| α1D-adrenoceptor (Human) | 90 | [35] |
| α2A-adrenoceptor (Human) | 256 | [35] |
| α2B-adrenoceptor (Human) | 24 | [35] |
| α2C-adrenoceptor (Human) | 353 | [35] |
| Calmodulin (Human) | 60000 | [36][35][37] |
| Calmodulin (Bovine) | 50000 | [36][37][35] |
| Chloroquine resistance transporter (Plasmodium falciparum) | 85000 | [38][35] |
| D1 receptor (Human) | 1372 | [35] |
| D2 receptor (Human) | 260 | [35] |
| D3 receptor (Human) | 190 | [35] |
| H1 receptor (Human) | 0.33[35]-1.4[39] | [39][35] |
| H2 receptor (Human) | 1146 | [35] |
| M1 receptor (Human) | 3.32 | [35] |
| M2 receptor (Human) | 12 | [35] |
| M3 receptor (Human) | 4.15 | [35] |
| M4 receptor (Human) | 1.06 | [35] |
| M5 receptor (Human) | 3.31 | [35] |
| NET (Human) | 4203 | [35] |
| Prion protein (Human) | 8000 | [40][35] |
| 5-HT1A receptor (Rat) | 1484 | [35] |
| 5-HT2A receptor (Human) | 19 | [35] |
| 5-HT2B receptor (Human) | 43 | [35] |
| 5-HT2C receptor (Human) | 6.48 | [35] |
| 5-HT6 receptor (Human) | 1128 | [35] |
| SERT (Serotonin transporter) (Human) | 2130 | [35] |
| Sigma1 receptor (Human) | 120 | [35] |
| OCT1 (Human) | 35100 | [41][35] |
Chemistry
editSolid promethazine hydrochloride is a white to faint-yellow, practically odorless, crystalline powder. Slow oxidation may occur upon prolonged exposure to air, usually causing blue discoloration. Its hydrochloride salt is freely soluble in water and somewhat soluble in alcohol. Promethazine is a chiral compound, occurring as a mixture of enantiomers.[42]
History
editPromethazine was first synthesized by a group at Rhone-Poulenc (which later became part of Sanofi) led by Paul Charpentier in the 1940s.[43] The team was seeking to improve on diphenhydramine; the same line of medical chemistry led to the creation of chlorpromazine.[44]
Society and culture
editAs of July 2017, it is marketed under many brand names worldwide: Allersoothe, Antiallersin, Anvomin, Atosil, Avomine, Closin N, Codopalm, Diphergan, Farganesse, Fenazil, Fenergan, Fenezal, Frinova, Hiberna, Histabil, Histaloc, Histantil, Histazin, Histazine, Histerzin, Lenazine, Lergigan, Nufapreg, Otosil, Pamergan, Pharmaniaga, Phenadoz, Phenerex, Phenergan, Phénergan, Pipolphen, Polfergan, Proazamine, Progene, Prohist, Promet, Prometal, Prometazin, Prometazina, Promethazin, Prométhazine, Promethazinum, Promethegan, Promezin, Proneurin, Prothazin, Prothiazine, Prozin, Pyrethia, Quitazine, Reactifargan, Receptozine, Romergan, Sominex, Sylomet, Xepagan, Zinmet, and Zoralix.[1]
It is also marketed in many combination drug formulations:
- with carbocisteine as Actithiol Antihistaminico, Mucoease, Mucoprom, Mucotal Prometazine, and Rhinathiol;
- with paracetamol (acetaminophen) as Algotropyl, Calmkid, Fevril, Phen Plus, and Velpro-P;
- with paracetamol and dextromethorphan as Choligrip na noc, Coldrex Nočná Liečba, Fedril Night Cold and Flu, Night Nurse, and Tachinotte;
- with paracetamol, phenylephrine, and salicylamide as Flukit;
- with dextromethorphan as Axcel Dextrozine and Hosedyl DM;
- with dextromethorphan and ephedrine as Methorsedyl;
- with dextromethorphan and pseudoephedrine as Sedilix-DM;
- with dextromethorphan and phenylephedrine as Sedilix-RX;
- with pholcodine as Codo-Q Junior and Tixylix;
- with pholcodine and ephedrine as Phensedyl Dry Cough Linctus;
- with pholcodine and phenylephedrine as Russedyl Compound Linctus;
- with pholcodine and phenylpropanolamine as Triple 'P';
- with codeine as Kefei and Procodin;
- with codeine and ephedrine as Dhasedyl, Fendyl, and P.E.C.;
- with ephedrine and dextromethorphan as Dhasedyl DM;
- with glutamic acid as Psico-Soma, and Psicosoma;
- with noscapine as Tussisedal; and
- with chlorpromazine and phenobarbital as Vegetamin.[1]
Recreational use
editThe recreational drug lean, also known as purple drank among other names, often contains a combination of promethazine with codeine-containing cold medication.[5]
Product liability lawsuit
editIn 2009, the US Supreme Court ruled on a product liability case involving promethazine. Diana Levine, a woman with a migraine, was administered Wyeth's Phenergan via IV push. The drug was injected improperly, resulting in gangrene and subsequent amputation of her right forearm below the elbow. A state jury awarded her $6 million in punitive damages.
The case was appealed to the Supreme Court on grounds of federal preemption and substantive due process.[45] The Supreme Court upheld the lower courts' rulings, stating that "Wyeth could have unilaterally added a stronger warning about IV-push administration" without acting in opposition to federal law.[46] In effect, this means drug manufacturers can be held liable for injuries if warnings of potential adverse effects, approved by the US Food and Drug Administration (FDA), are deemed insufficient by state courts.
In September 2009, the FDA required a boxed warning be put on promethazine for injection, stating the contraindication for subcutaneous administration. The preferred administrative route is intramuscular, which reduces risk of surrounding muscle and tissue damage.[47]
References
edit- ^ a b c d "Promethazine international brands". Drugs.com. Retrieved 17 July 2017.
- ^ a b c d Strenkoski-Nix LC, Ermer J, DeCleene S, Cevallos W, Mayer PR (August 2000). "Pharmacokinetics of promethazine hydrochloride after administration of rectal suppositories and oral syrup to healthy subjects". American Journal of Health-System Pharmacy. 57 (16): 1499–505. doi:10.1093/ajhp/57.16.1499. PMID 10965395.
- ^ Paton DM, Webster DR (1985). "Clinical pharmacokinetics of H1-receptor antagonists (the antihistamines)". Clinical Pharmacokinetics. 10 (6): 477–97. doi:10.2165/00003088-198510060-00002. PMID 2866055. S2CID 33541001.
- ^ a b c d e f g h i j k l m n "Promethazine Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 24 October 2018.
- ^ a b Agnich LE, Stogner JM, Miller BL, Marcum CD (September 2013). "Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures" (PDF). Addictive Behaviors. 38 (9): 2445–9. doi:10.1016/j.addbeh.2013.03.020. PMID 23688907.
- ^ a b British national formulary : BNF 74 (74 ed.). British Medical Association. 2017. p. 276. ISBN 978-0-85711-298-9.
- ^ Malamed SF (2009). Sedation: A Guide to Patient Management. Elsevier Health Sciences. p. 113. ISBN 978-0-323-07596-1.
- ^ Page CB, Duffull SB, Whyte IM, Isbister GK (February 2009). "Promethazine overdose: clinical effects, predicting delirium and the effect of charcoal". QJM. 102 (2): 123–131. doi:10.1093/qjmed/hcn153. PMID 19042969. S2CID 17677540.
- ^ Li JJ (2006). Laughing Gas, Viagra, and Lipitor: The Human Stories behind the Drugs We Use. United Kingdom: Oxford University Press. p. 146. ISBN 978-0-19-988528-2. Retrieved 9 July 2016.
- ^ a b "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Promethazine Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ "Dextromethorphan; Promethazine Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ a b c d e f g h i j k l m n Southard BT, Al Khalili Y (2019). "Promethazine". StatPearls. PMID 31335081. This article incorporates text available under the CC BY 4.0 license.
- ^ "Promethazin - Anwendung, Wirkung, Nebenwirkungen | Gelbe Liste". Gelbe Liste Online (in German). Retrieved 22 May 2023.
- ^ British National Formulary (March 2001). "4.6 Drugs used in nausea and Vertigo - Vomiting of pregnancy". BNF (45 ed.)..
- ^ "Rhea Seddon Oral History". NASA Johnson Space Center Oral History Project. 10 May 2011. Retrieved 25 May 2021.
- ^ "Promethazine (Phenergan)". Medicines A to Z. National Health Service. 27 October 2021. Archived from the original on 3 August 2023. Retrieved 2 October 2023.
- ^ Schreiner NM, Windham S, Barker A (December 2017). "Atypical Neuroleptic Malignant Syndrome: Diagnosis and Proposal for an Expanded Treatment Algorithm: A Case Report". A&A Case Reports. 9 (12): 339–343. doi:10.1213/XAA.0000000000000610. PMID 28767476. S2CID 39699580.
- ^ National Institute for Health and Care Excellence
- ^ Hampton T (23 February 2005). "Promethazine Warning". JAMA. 293 (8): 921. doi:10.1001/jama.293.8.921-c.
- ^ "Cordingley Neurology". Archived from the original on 21 December 2016. Retrieved 15 February 2008.
- ^ NCQA's HEDIS Measure: Use of High Risk Medications in the Elderly Archived 1 February 2010 at the Wayback Machine
- ^ Starke P, Weaver J, Chowdhury B (2005). "Boxed warning added to promethazine labeling for pediatric use". N. Engl. J. Med. 352 (5): 2653. doi:10.1056/nejm200506233522522. PMID 15972879.
- ^ Salahudeen MS, Duffull SB, Nishtala PS (March 2015). "Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review". BMC Geriatrics. 15 (31): 31. doi:10.1186/s12877-015-0029-9. PMC 4377853. PMID 25879993.
- ^ a b c d e "Phenergan" (PDF). www.accessdata.fda.gov. Retrieved 30 September 2023.
- ^ "promazine | Ligand Activity Charts | IUPHAR/BPS Guide to PHARMACOLOGY". www.guidetopharmacology.org. Retrieved 18 May 2023.
- ^ Möller HJ, Müller WE, Bandelow B (2001). Neuroleptika – Pharmakologische Grundlagen, klinisches Wissen und therapeutisches Vorgehen (in German). Stuttgart: Wissenschaftliche Verlagsgesellschaft. ISBN 978-3-8047-1773-2.
- ^ Benkert O, Hippius H (1995). Psychiatrische Pharmakotherapie. doi:10.1007/978-3-642-79084-3. ISBN 978-3-540-58149-9.
- ^ Hill SJ, Young M (December 1978). "Antagonism of central histamine H1 receptors by antipsychotic drugs". European Journal of Pharmacology. 52 (3–4): 397–399. doi:10.1016/0014-2999(78)90297-2. PMID 32056.
- ^ a b Fiorella D, Rabin RA, Winter JC (October 1995). "The role of the 5-HT2A and 5-HT2C receptors in the stimulus effects of hallucinogenic drugs. I: Antagonist correlation analysis". Psychopharmacology. 121 (3): 347–56. doi:10.1007/bf02246074. PMID 8584617. S2CID 24420080.
- ^ Seeman P, Watanabe M, Grigoriadis D, et al. (November 1985). "Dopamine D2 receptor binding sites for agonists. A tetrahedral model". Molecular Pharmacology. 28 (5): 391–9. PMID 2932631. Archived from the original on 29 August 2021. Retrieved 28 November 2011.
- ^ Burt DR, Creese I, Snyder SH (April 1977). "Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain". Science. 196 (4287): 326–8. Bibcode:1977Sci...196..326B. doi:10.1126/science.847477. PMID 847477.
- ^ a b Prasad JP (2010). Conceptual Pharmacology. Universities Press. pp. 295, 303, 598. ISBN 978-81-7371-679-9. Retrieved 27 November 2011.
- ^ a b Adolph O, Köster S, Georgieff M, Georgieff EM, Moulig W, Föhr KJ (August 2012). "Promethazine inhibits NMDA-induced currents - new pharmacological aspects of an old drug". Neuropharmacology. 63 (2): 280–291. doi:10.1016/j.neuropharm.2012.03.006. PMID 22507664. S2CID 35487146.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad "promethazine | Ligand Activity Charts | IUPHAR/BPS Guide to PHARMACOLOGY". www.guidetopharmacology.org. Retrieved 18 May 2023.
- ^ a b Bruno C, Cavalluzzi MM, Rusciano MR, Lovece A, Carrieri A, Pracella R, et al. (June 2016). "The chemosensitizing agent lubeluzole binds calmodulin and inhibits Ca(2+)/calmodulin-dependent kinase II". European Journal of Medicinal Chemistry. 116: 36–45. doi:10.1016/j.ejmech.2016.03.045. PMID 27043269.
- ^ a b Bolshan Y, Getlik M, Kuznetsova E, Wasney GA, Hajian T, Poda G, et al. (March 2013). "Synthesis, Optimization, and Evaluation of Novel Small Molecules as Antagonists of WDR5-MLL Interaction". ACS Medicinal Chemistry Letters. 4 (3): 353–357. doi:10.1021/ml300467n. PMC 4027439. PMID 24900672.
- ^ Deane KJ, Summers RL, Lehane AM, Martin RE, Barrow RA (May 2014). "Chlorpheniramine Analogues Reverse Chloroquine Resistance in Plasmodium falciparum by Inhibiting PfCRT". ACS Medicinal Chemistry Letters. 5 (5): 576–581. doi:10.1021/ml5000228. PMC 4027738. PMID 24900883.
- ^ a b Nakai T, Kitamura N, Hashimoto T, Kajimoto Y, Nishino N, Mita T, et al. (August 1991). "Decreased histamine H1 receptors in the frontal cortex of brains from patients with chronic schizophrenia". Biological Psychiatry. 30 (4): 349–356. doi:10.1016/0006-3223(91)90290-3. PMID 1912125. S2CID 9715772.
- ^ Vogtherr M, Grimme S, Elshorst B, Jacobs DM, Fiebig K, Griesinger C, et al. (August 2003). "Antimalarial drug quinacrine binds to C-terminal helix of cellular prion protein". Journal of Medicinal Chemistry. 46 (17): 3563–3564. doi:10.1021/jm034093h. PMID 12904059.
- ^ Ahlin G, Karlsson J, Pedersen JM, Gustavsson L, Larsson R, Matsson P, et al. (October 2008). "Structural requirements for drug inhibition of the liver specific human organic cation transport protein 1". Journal of Medicinal Chemistry. 51 (19): 5932–5942. doi:10.1021/jm8003152. PMID 18788725.
- ^ "RxList: Promethazine Description". 21 June 2007. Archived from the original on 11 September 2008. Retrieved 4 June 2008.
- ^ Ban TA (2006). "The role of serendipity in drug discovery". Dialogues in Clinical Neuroscience. 8 (3): 335–44. doi:10.31887/DCNS.2006.8.3/tban. PMC 3181823. PMID 17117615.
- ^ "Paul Charpentier, Henri-Marie Laborit, Simone Courvoisier, Jean Delay, and Pierre Deniker". Science History Institute. 6 August 2015. Archived from the original on 20 March 2018. Retrieved 20 March 2018.
- ^ Liptak A (18 September 2001). "Drug Label, Maimed Patient and Crucial Test for Justices". The New York Times. Retrieved 31 October 2008.
- ^ Stout D (4 March 2009). "Drug Approval Is Not a Shield From Lawsuits, Justices Rule". The New York Times. Retrieved 4 March 2009.
- ^ "Information for Healthcare Professionals: Intravenous Promethazine and Severe Tissue Injury, Including Gangrene". Food and Drug Administration. 15 August 2013.